Breastfeeding, AKA nursing, can be a beautiful way to bond with your baby. But like all relationships, breastfeeding can also be fraught: difficult, painful, emotional, and confusing. Here are some lesser-known breastfeeding FAQs to help you understand what to expect. After all, there are many facts about breastfeeding that aren’t common knowledge, even among pregnant women and new mothers.
These breastfeeding FAQs will help clear up misconceptions and give you more info to chat about with your doctor, lactation consultant, or doula. We’ve got plenty of other pieces on the Mothership to unpack some of your other burning questions. Head here for more.
Can I breastfeed or pump with breast implants or reduction surgery?
Yes! According to Johns Hopkins Medicine, women with breast implants or reductions can still breastfeed. Breast augmentation does not interfere with the mammary glands and ducts where milk is produced. That’s because implants are placed between the chest wall and breast, so they’re not getting in the mix with your mammary ducts. That doesn’t necessarily mean that those ducts will produce enough; plenty of women without breast surgery have supply issues. And in some cases, implants may reduce the amount of milk produced or restrict flow. Depending on how you’ve healed and where your scar is, you may experience some nerve issues that can impact letdown. Lactation consultants can help with this.
If you’ve got implants, you might also worry that the chemicals from the implant might harm your baby. If you have saline implants, the general consensus is that it’s fine for saline water to mix with breast milk. Other breast implants contain silicone, but this is unlikely to leach into your milk. Talk to your doctor and lactation consultant for more info.
In breast reduction surgery, some glandular tissue is removed, which would impact supply, but still enable you to breastfeed or pump successfully.
Should I breastfeed while I’m sick? What about when my baby is sick?
Generally speaking, yes!
Now, that answer gets a bit more qualified if your baby is less than three weeks or was premature and if you have a more serious illness. If you’re taking medications, you’ll want to run them by your doctor or the baby’s pediatrician to make sure they’re compatible with breastfeeding.
When you breastfeed—or pump—your body acts as your baby’s personal pharmacy. Writing for Parents magazine, Dr. Catherine Dundon explains that mothers pass antibodies—which are targeted against pathogens in the family’s immediate surroundings—to their babies via breast milk. Because you’ll begin producing antibodies 12–24 hours before you actually feel symptoms, chances are that your baby will become immune before catching anything. Likewise, breast milk is rich with immune cells—white blood cells, or leukocytes—to ward off infection. Magic!
If your baby is sick, continue to breastfeed. Breastfeeding will help your baby recover faster by providing optimal nutrition as well as white blood cells, stem cells, and protective enzymes.
What skincare products are safe to use while breastfeeding?
The following skincare products are safe to use while breastfeeding: gentle soap and facial cleansers, most moisturizers, and most natural/chemical-free products. Avoid products that contain vitamin A (retinol or retinoid), hydroquinone, salicylic acid, and benzoyl peroxide.
As with all breastfeeding FAQs, always talk to your doctor or lactation consultant before beginning any new medication or introducing a new chemical product into your body.
When will my milk come in?
Although every mom is different, most women begin producing colostrum while pregnant around 16–22 weeks. There’s some evidence that suggests that early hand expression of colostrum can help with production later on. You can learn how to do that here.
Colostrum is what your newborn will consume at birth. The colostrum transitions to mature milk approximately two to five days after your baby is born.
Breastfeeding newborns: What should I expect?
Every baby is different, so your experience breastfeeding a newborn will be unique. Conventional wisdom is that in those early days, babes feed a lot more than you expect them to: They eat every two hours, and some sleepy or cuddly babies spend a while at the breast. But if you’re worried, want reassurance, or need tips to make your routine work for both of you, talk to a lactation consultant. Find one at The Motherlode.
Which medicine can I take while breastfeeding?
Many common medications haven’t been tested for their impact on breastfeeding babies. That would be a risky study to run! However, the following over-the-counter medicines are generally thought to be safe: Tylenol (acetaminophen), Maalox, Mylanta, TUMS, Gaviscon, Riopan, Titralac, Neosporin, Bacitracin, and J & J.
Always consult your physician before starting a new prescription medication while breastfeeding. To learn more, see our article: Which medications are safe while pregnant?
What foods/drinks should I avoid while breastfeeding? What impact does my diet have on breastfeeding?
To understand how breastmilk is affected by things you ingest or put on your skin, consider how breastmilk is made: The hormone prolactin signals to your bod that it’s time to make milk, and then the alveoli take proteins, sugars, and fat from your blood supply and make breastmilk. So when we talk about skincare that’s breastfeeding-safe, the key consideration is whether it’s absorbed by the blood through the skin—or else is applied near enough to your babe to get on him or her.
The same principles apply for food and drink.
For drinks, limit your alcohol intake. Alcohol is all about your BAC, and generally speaking the alcohol content in your blood will peak after about 40 minutes. It depends on height and weight, but the body generally metabolizes alcohol at the rate of one drink per two hours. So if you plan to drink, wait two hours per drink before breastfeeding. The old conventional wisdom around “pumping and dumping” doesn’t quite apply in the way we used to think it did. It’s less important to pump in order to rid the body of “contaminated milk,” because you can often wait it out. Instead, you might choose to pump and dump while drinking simply to keep up your supply while you aren’t actually feeding.
Similarly, experts recommend that you limit caffeine intake, too, as that goes into the bloodstream. You can choose what’s right for you, but many experts say two cups of coffee (or other caffeinated beverages) per day is a good rule of thumb.
On the food front, eating a nutritious diet is a good idea in general. But you’ll find mixed word on whether certain foods affect the flavor of your breast milk or can make your baby fussy or gassy. The idea that baby’s fussiness and gassiness can be caused by something mom ate is super persistent, but there’s no research to back it up: It’s something like an old wives’ tale. As KellyMom puts it:
There are NO foods that a mother should avoid simply because she is breastfeeding. It is generally recommended that you eat whatever you like, whenever you like, in the amounts that you like and continue to do this unless you notice an obvious reaction in your baby to a particular food.
Eating certain foods may cause gas in mom due to the normal breakdown of some of the undigested carbohydrates (sugar, starches, soluble fiber) by bacteria in the large intestine (see Gas in the digestive tract).
However, breastmilk is made from what passes into mom’s blood, not what is in her stomach or digestive tract. Neither the gas nor the undigested carbohydrates (whose breakdown can cause gas in mom) pass into mom’s blood, so it is impossible for these things to pass into your milk to make your baby gassy.
The only hard and fast rule is that you should not diet and should drink plenty of water.
Can I lose weight while breastfeeding?
The season of postpartum is difficult, and body image can exacerbate it. But it’s important to be patient, and dieting is generally not advised while breastfeeding. Breastfeeding mothers can expect to lose one to two pounds a month by breastfeeding alone, simply because it takes so much energy to make all that milk. For losing extra weight via diet and exercise, experts recommend waiting between six to eight weeks after your baby is born before you make any changes. This will give your body time to recover and help you establish a balanced milk-production/breastfeeding routine.
What is the best breastfeeding position?

Any position where your baby is able to “latch” and you’re both comfortable will be the best breastfeeding position for you. If you can’t master the football hold, don’t sweat it! It’s about what works for your baby and you. If you’re having trouble, a lactation consultant can help you find the best position. To learn more about this and other breastfeeding FAQs about positioning, see our article: The best breastfeeding positions for mom and baby.
How can I increase my breast milk?
Over at KellyMom, lactation consultant Kelly Bonyata explains that many women who fear they have a low supply of breast milk are actually producing at normal levels. As long as your baby is gaining weight and needs a normal number of diaper changes, your breast milk is fine. But it’s hard to know, and the amount you pump may not be a 1:1 comparison. If you want some confirmation and insight, we recommend working with a lactation consultant, who will watch your feeds, offer advice, and weigh your baby to determine how much they’re getting.
However, if you need to increase your breast milk, try the following: offer both breasts equally and switch sides more often during feeding, nurse more frequently, give the baby breast milk only, consider pumping, and talk to your lactation consultant.
How often should I breastfeed?
For the first month, a newborn should feed 8–12 times per day. By one to two months, this should decrease slightly to seven to nine times per day. As your baby gets older, their feeding schedule will change and your unique breastfeeding pattern will emerge. Some babies breastfeed more often than others. However, KidsHealth.org explains that newborns shouldn’t go longer than four hours without breastfeeding. Your pediatrician can tell you more about what to expect for your particular baby.
How do I know if my baby is getting enough milk?
Rest assured that your baby is getting enough milk as long as they are nursing frequently, gaining weight, and showing signs of overall health, such as peaceful sleep and alertness while awake. A baby that gets enough milk will also require at least six diaper changes per day, including three to four bowel movements by four days of age.
Who can help me with breastfeeding?
If you need help with breastfeeding, seek out a lactation consultant. Lactation consultants are trained experts who act as breastfeeding coaches. A lactation consultant can provide a variety of services, from simply answering questions to helping you find a proper nursing position. Check out the Motherlode for our directory of LCs!
How do I find a lactation specialist?
There are several ways to find a lactation consultant. Ask for recommendations from the hospital or birthing center where you delivered, talk to other parents in your parenting group or class, or search an online directory such as Motherfigure’s Motherlode or the International Lactation Consultant Association.
Tips for breastfeeding when you go back to work
First, talk to your HR department to learn about your company’s policies for accommodating breastfeeding. Then, establish a pumping routine before you return to work. Parenting website TinyHood recommends setting a schedule based around your baby’s feeding habits. You can also begin freezing your milk before you go back to work, building up a “milk stash.” Finally, talk to your baby’s caregiver and communicate a plan for bottle feeding.
How do I know if I have mastitis?
Mastitis, or inflammation of the breast, will be very painful. You may experience some of these common signs and symptoms: pain or burning sensation while breastfeeding, breast soreness or swelling, tender breasts, a rash, and flu-like symptoms. For more, see our article: Mastitis breastfeeding: How to deal with mastitis while breastfeeding.
Breastfeeding is difficult for me. Is it OK to stop?
Yes. However, experts caution against stopping immediately. Abrupt weaning can lead to complications such as plugged ducts and mastitis. Stopping too quickly can also cause discomfort or pain.
How soon should I start breastfeeding after birth?
Experts agree that you should begin breastfeeding as soon as possible. Ideally, begin breastfeeding within the first hour of postpartum.
Can I drink alcohol/caffeine while breastfeeding?
Yes, but for alcohol, wait two hours per drink before breastfeeding (or breastfeed/pump before drinking). For caffeine, about two cups of coffee (or other caffeinated beverages) is the general recommendation, and you may find that more or less works for you.
My nipples are sore and cracked. What can I do?
There are several remedies for sore, cracked nipples. Healthline recommends applying a warm compress, smoothing fresh milk onto the nipple, using a homemade saltwater rinse, or using lanolin ointment. It’s also recommended to change nursing pads more frequently if you are experiencing nipple irritation.
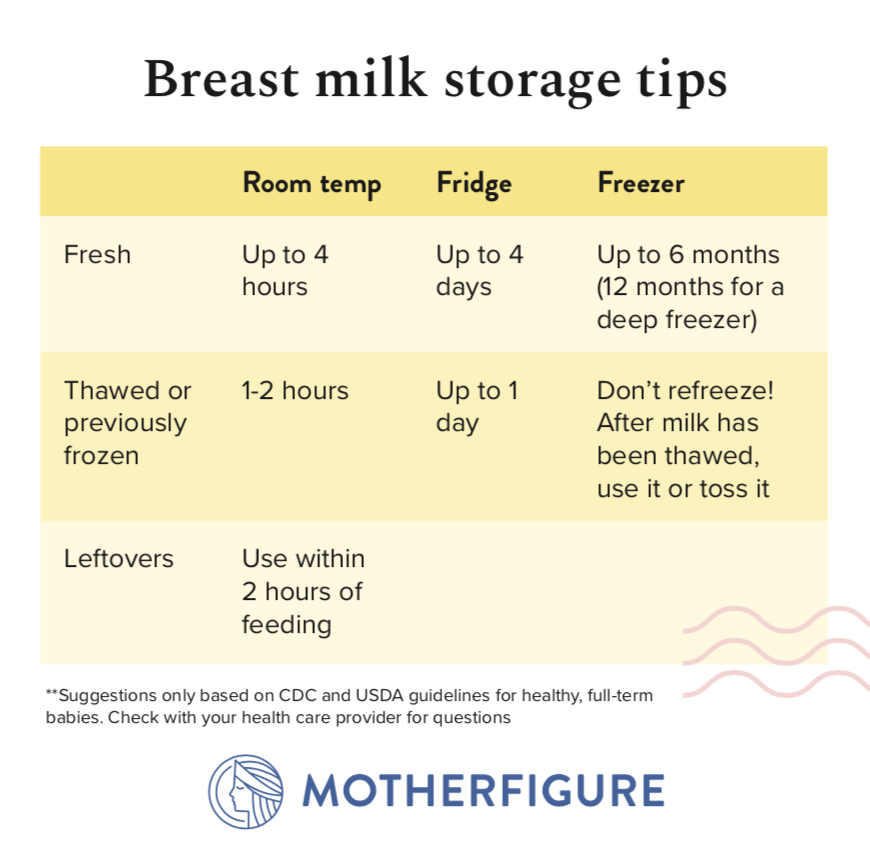
How should I store breast milk?
According to WomensHealth.gov, there are several ways to store breast milk. At room temperature (up to 77° F), breast milk can be stored for up to four hours. It can be refrigerated up to four days and frozen within four days of pumping. Use breast milk storage bags, clean glass, or air-tight, hard plastic, BPA-free containers.
How often should I alternate breasts?
In general, you should give your baby equal time feeding from each breast. Many experts recommend switching from one breast to the other when you’re halfway through a feeding session. But if babe seems to prefer one breast? That’s OK! There aren’t long-term problems associated with that, and many women have successfully breastfed using only one breast.
How long should I breastfeed my baby?
This is a personal decision. Every mother and baby is different, and there may be medical reasons that dictate when you need to wean. But if you’re looking for the general guidance from the World Health Organization and the American Academy of Pediatrics, they recommend breastfeeding for at least the first year.
How can I prevent my teething baby from biting while breastfeeding?
La Leche League International advises mothers to prevent biting by ensuring a correct latch and proper positioning. When positioned right, a teething baby won’t be able to bite because they’ll be actively sucking and swallowing. You might still get some scrapes, but you can break the latch by putting your finger in the side of your baby’s mouth and trying again.
Does breastfeeding impact fertility?
Most women do not menstruate while breastfeeding, a phase known as lactational amenorrhea. According to KellyMom, exclusive breastfeeding is 98–99.5 percent effective as a method of birth control. However, this changes once the baby begins eating solid foods, your period returns, or other factors.
How do I wean?
To wean, the Mayo Clinic recommends women slowly taper daily breastfeeding. Gradually reduce time spent breastfeeding as well as the frequency of feedings. This will cause your body to begin reducing its milk production without causing engorgement or other complications. Depending on your body and your baby, weaning can occur over weeks or it can take months.
Are you a first-time mom looking for even more tips? Check out this article: Breastfeeding tips for first–time moms.
