When my husband and I were ready to start a family, we were really ready. Like many prospective first-time parents, we assumed that ditching birth control led to a baby roughly nine months later. But that’s not what happened. We tried, and tried, and tried some more. After two years of infertility and invasive treatments, I finally got pregnant—but I found that I wasn’t able to enjoy my pregnancy because of the infertility I had endured.
By the time I hit my mid 20s, I was a seasoned overachiever. Naturally, after several cycles without a coveted BFP, I decided to up my game and became an extreme ovulation monitor. Everything became structured, and spontaneity flew out the window. Obsessing over ovulation is far from glamorous, especially the baby-making part, but even adhering to a strict regimen didn’t yield a positive pregnancy test. The scientist in me, the one that taught reproductive health classes to teenagers at the health department, tried to hold on to logic. While I knew it was possible to get pregnant the very first time sans birth control, that was a bit of an oversimplification. I continued to tell myself that once I was pregnant, surely all this work would allow me to revel in the antenatal glow depicted in movies, TV, and social media.
My OB-GYN, whom I’d informed of my procreative intentions, initially waved me off with the assurance that conception was imminent, I just needed to “relax” and “take my time.” The youthfulness of my eggs (I was 26 at the time) would surely come to baby fruition in a matter of cycles. But just in case, she’d set up a pelvic ultrasound at my request. By the time I got that ultrasound, my husband and I had been trying for a full year. Each cycle, I’d end up overanalyzing every little cramp and feeling of nausea, driving myself crazy with attempting to manifest positives that were simply not there. Yet, I waited. Partly because I was confident I would be pregnant by then. More practically, however, that was when my insurance would start to foot some of the bill—once I had an official infertility diagnosis in hand.
I continued to tell myself that once I was pregnant, surely all this work would allow me to revel in the antenatal glow depicted in movies, TV, and social media.
After the ultrasound, I went back to that OB-GYN, who this time matter-of-factly diagnosed me with polycystic ovarian syndrome (PCOS). She said I likely wasn’t ovulating at all, at least not with a truly viable egg. No matter how optimized our attempts had been, if I wasn’t actually releasing an egg (anovulation), it wouldn’t be fertilized by sperm and I wouldn’t get pregnant. In addition, my transvaginal ultrasound had revealed a number of polyps (another common finding in women with PCOS), one of which was either on my cervix or really close to it.
I was crushed and confused. The last time I visited this doctor, she had given me her assurances that everything was fine. It’s not like this was our first communication in the last year, what with my emailing the office almost monthly. Why didn’t she warn me about this? Before that moment, I never thought about what it would mean to intentionally seek out reproductive help. Now my husband, the engineering fixer, and I, the biologist, would need intentional help to start our family. Theoretically, I knew how invasive this could get and my mind immediately went to IVF: shots of hormones, egg retrievals, more doctor’s appointments, more waiting, more hope that may never manifest. I knew I’d be willing to try, but would my husband? That discussion hadn’t happened. Even as a genetic scientist, I know that genes are not the end-all be-all of a family. But I also know the journey is incredibly difficult, both physically and emotionally.
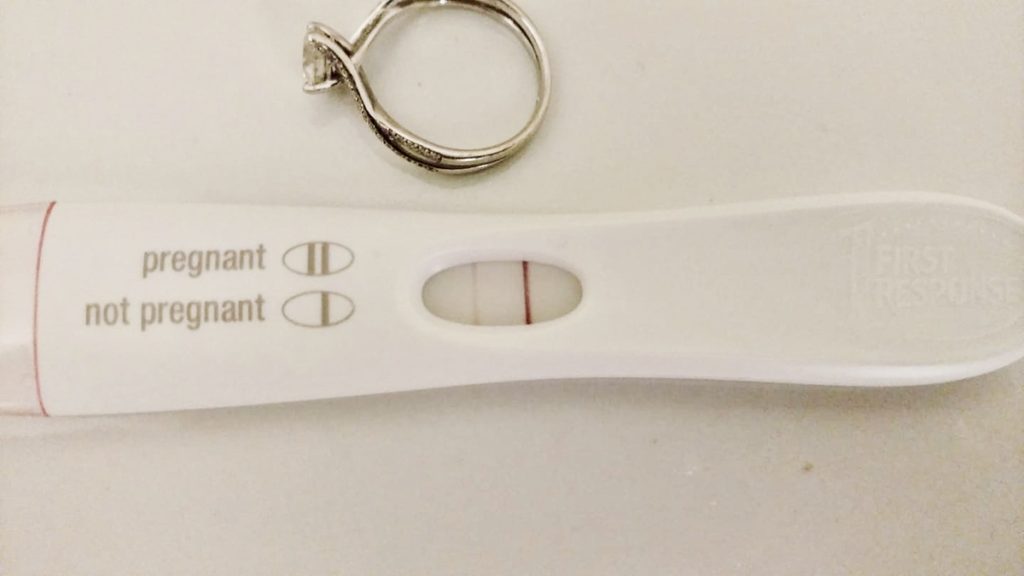
I had a surgery to remove the polyps, and consulted a reproductive endocrinologist who started me on a low dose of letrozole, which would hopefully lower my estrogen levels enough to allow for proper ovulation. I was relieved we wouldn’t have to jump to IVF yet. The doctor closely monitored the follicular growth of my eggs throughout my cycle, which meant many trips to the clinic. Several attempts and a dosage increase later, I successfully ovulated! I couldn’t make it through the full two-week wait, so nine days later I took a pregnancy test. And there they were: two beautiful lines. I was pregnant.
Immediately, I felt a rush of emotions: elation, relief, excitement. The two years leading up to this moment now felt productive. While I began dreaming about our family’s future, I also knew this was only the beginning. I had hoped that now, finally, I’d be able to enjoy this path to parenthood—but I also felt a nervousness that was hard to shake. I told myself if I could get this far, everything would work out, but I didn’t really believe it.
My day job was analyzing chromosomes. I was extremely well versed in prenatal genetics and the outcomes and statistics associated with early pregnancy loss. In addition, the online infertility support group I’d joined exposed me to the painful experiences of early pregnancy loss that are all too common in the infertility community.
I told myself if I could get this far, everything would work out, but I didn’t really believe it.
At the six-week ultrasound, my husband clenched my hand as we waited for the tech to find not only a gestational sac but a heartbeat. And then, we heard it: a strong and quick heartbeat that made the last two years worth it. Tears of joy rolled down my face.
At 12 weeks we dutifully announced to the world that we were with child via a clever Facebook post. I, cautiously, felt like I was starting to get comfortable with the pregnancy and that things might just work out all right. Even though I was puking most mornings, I started looking forward to seeing my belly grow, feeling baby kick flutters, and arguing with my husband over baby names.
Then I hit 14 weeks’ gestation, and I started bleeding. Any bright, red blood would concern a pregnant mom, but the amount of blood I experienced was truly terrifying. I was convinced I was losing my baby. I had become too comfortable, too soon, and now it was ending. My husband rushed me to the ER, where I was told fairly tersely, “Since you’re only 14 weeks, there’s really not much we can do.” Given my scientific background, I knew this all too well— but surely a medical professional should have a kinder way of relaying that information.
I was readying myself for the worst when, on the ultrasound, I saw my baby was perfectly content. Heartbeat still strong, seemingly unfazed by the current situation. I cried. Moreover, I sobbed with the knowledge that it wasn’t over. It felt like a second chance. The official diagnosis was a subchorionic hematoma, and I was told to avoid heavy lifting and scheduled an early checkup a few weeks later.
The succeeding months were full of anxiety as I waited for something bad to happen. Similar to when I was trying to get pregnant, I now overanalyzed every little pain and symptom to the point of obsession. My new goal was to get to viability (about 25 weeks). Once I got there, I told myself, then I could relax and enjoy my pregnancy. Until then, I bought myself a fetal doppler and would listen for a heartbeat every morning when I woke up, just in case.
My obsessive tracking of ovulation in my infertility journey was now an ever-present part of my pregnancy. I wanted to enjoy the journey, but I was scared.
But even after I reached viability, I still worried about kick counts and fetal activity. Each doctor’s visit was checked off the list as one step closer to getting to baby. I had imagined myself living in excited anticipation, when in reality it was more nervous anxiety. I look back and think I should have relished particular moments a little more, like when we found out we were having a girl. Instead, I paid close attention to her frequency of hiccups and whether she was flipping often enough. My obsessive tracking of ovulation in my infertility journey was now an ever-present part of my pregnancy. I wanted to enjoy the journey, but I was scared. Of course, there were still times of joy during the pregnancy, like at my work’s baby shower. However, I remained on constant alert, waiting for the next potential calamity to come our way. I wanted to be “Instagram happy” throughout my pregnancy, but it just wasn’t in the cards for me.
My labor was quick and uncomplicated, a true blessing. I opted out of pain medications, which meant my labor was fairly anxiety-free since all of my focus was working through contractions. Then, after one last wave of power, she was earthside. I was overcome with relief, physically and emotionally. She made it. We did it. I held her on my chest, staring down at her, and finally stopped holding my breath.
Like this piece? Subscribe to our newsletter for real stories about women on their journey to motherhood.
